How to Recognize and Treat Internal Hemorrhoids?
Internal hemorrhoids are one of those topics that people rarely discuss openly, usually due to the discomfort associated with their location and symptoms.
Many people live with Internal Hemorrhoids for a long time without realizing what exactly causes them or how to deal with them. They are often confused with other conditions, and sometimes even ignored until they cause severe discomfort or serious complications.
In this article, we will look at what internal hemorrhoids are, what causes them, their symptoms, how long they last and how to treat them.
Table of Contents
1. What are Internal Hemorrhoids?
Internal hemorrhoids are part of the natural anatomy of the human body. Everyone has hemorrhoidal cushions - structures made up of connective tissue, blood vessels and smooth muscle located in the rectal area.
Problems arise when these cushions become enlarged and begin to cause discomfort. This enlargement may be related to increased pressure in the rectum, loss of elasticity in the tissues or weakening of the supporting muscles.
Unlike External hemorrhoids, Internal hemorrhoids are not located under the skin around the anus, but deeper under the lining of the rectum. In the early stages, they usually do not cause pain because there are fewer nerve endings in this area.
Internal hemorrhoids do not always develop linearly - they can remain in a mild stage for a long time and then suddenly become more severe, for example after physical exertion, illness or a sudden change in diet.
2. Causes of Internal Hemorrhoids
The causes of Internal hemorrhoids are not the same for every person. Both physical and genetic factors play a role.
Here are some of the factors that lead to the appearance of Internal Hemorrhoids:
Heredity
Some people are born with weaker venous walls or weaker connective tissue in the rectal area.
Genetic predisposition increases the likelihood of developing hemorrhoids at a young age.
Impaired circulation in the pelvis

Prolonged sitting, especially in a stationary position, leads to blood stagnation in the lower body.
This creates conditions for the veins in the rectum to dilate and form internal hemorrhoids.
Hormonal changes
In women, especially during pregnancy or menstruation, hormonal imbalance can cause the venous walls to relax.
This increases the risk of hemorrhoid problems even in the absence of other factors.
Low physical activity
A sedentary lifestyle leads to weakening of the abdominal and pelvic muscles.
This makes it difficult to defecate and increases internal pressure.
Incorrect toileting routine
Frequent stool retention due to lack of time or suitable conditions can lead to persistent constipation.
This creates a habit of straining during bowel movements which damages the rectal veins.

Stress and mental strain
Although it may sound surprising, chronic stress affects digestion and peristalsis.
When stressed, the body releases hormones that can disrupt normal bowel movements and cause cramps, bloating and constipation - indirect factors in the development of hemorrhoids.
Age
As we age, the elasticity of tissues decreases. Veins become more easily dilated and susceptible to pressure.
This is why Internal Hemorrhoids are more common after the age of 40.
3. What are the symptoms of Internal Hemorrhoids?
The symptoms of Internal Hemorrhoids can vary greatly depending on the stage of the condition and the individual sensitivity of the person. Sometimes they are almost imperceptible, while other times they cause serious discomfort.
1. Slight bleeding during bowel movements
Bleeding is the most commonly noticed symptom. Usually, a few drops of bright red blood are noticed on the toilet paper, in the toilet bowl or on the surface of the stool.
The color of the blood is important - with Internal Hemorrhoids it is always fresh, as it comes from superficial blood vessels, near the end of the rectum.
Many people are scared by the sight of blood, but hemorrhoids rarely cause a lot of bleeding. However, bleeding should not be ignored, as it can also be a symptom of other conditions such as an anal fissure or even colon cancer.
2. Itching and irritation in the anal area
This condition results from mucus discharge or slight leakage of fecal matter.
The mucous membrane that covers internal hemorrhoids can secrete a secretion that irritates the skin around the anus, especially when sitting for long periods of time or wearing tight clothing.
Itching often worsens at night or after a bowel movement. If a person starts scratching it can damage the skin and cause secondary infections or inflammation.

3. Sensation of incomplete bowel emptying
Many people with Internal Hemorrhoids report a feeling that their bowels have not completely emptied, even after a bowel movement.
This sensation is due to the physical presence of hemorrhoidal nodes in the rectal canal, which can create a "deceptive" feeling of residue.
This often causes sufferers to return to the toilet repeatedly, without any real need, which in turn contributes to even greater tension and worsening of the condition.
4. Heaviness or pressure in the rectal area
People describe this feeling as a “lump,” “pressure,” or “swelling” in the lower rectum.
This is especially noticeable after prolonged sitting, exercise or eating which causes the intestines to bulge.
This pressure is not pain, but rather discomfort, which over time can become intrusive and interfere with the normal rhythm of life.
5. Periodic protrusion of hemorrhoids outside the anus (prolapse)
As the condition progresses, internal hemorrhoids may "pop" out of the anus during bowel movements. At first, this only happens with strong straining and the nodes retract back on their own.
Over time, however, they may stay out longer, require manual retraction, and in the most severe cases, may not be able to go back in at all. Prolapse is a serious sign of deterioration and often requires medical intervention.
6. Mucus leakage
Mucus is a sticky, colorless or slightly yellowish fluid that is secreted from the lining of the internal hemorrhoids and can leak through the anus, especially when walking, straining, or after a bowel movement.
Leakage leads to a feeling of wetness, stickiness, and sometimes an unpleasant odor, which creates social discomfort and makes personal hygiene difficult.
7. Frequent urge to defecate (tenesmus)
Even though the bowels are already empty, the presence of enlarged hemorrhoids in the rectum can convince us that we need to visit the toilet.
This condition is called tenesmus. It leads to repeated but unsuccessful attempts to defecate and additional straining that worsens the condition and can cause bleeding or prolapse.
8. Mild pain or discomfort (in later stages)

While the early stages of Internal Hemorrhoids do not cause pain, complications may cause burning, dull, sharp or stabbing pain.
This usually happens when there is:
- Hemorrhoid impingement outside the anus;
- Inflammation;
- Development of a thrombus (blood clot).
Then the symptoms become more severe and often medical treatment or even surgery is required.
9. Increased sensitivity in the rectal area
Some people experience an uncomfortable "pins and needles," tightness, or even pain when sitting, especially on hard surfaces. It becomes difficult to sit still for long periods of time.
In other cases, even washing after using the toilet causes unpleasant sensations, and wearing tight underwear or clothing further worsens the condition.
These symptoms can occur individually or in combination. Sometimes they occur intermittently, and in other cases - constantly.
It is important to pay attention to even mild signs to avoid hemorrhoids progressing to a more severe form.
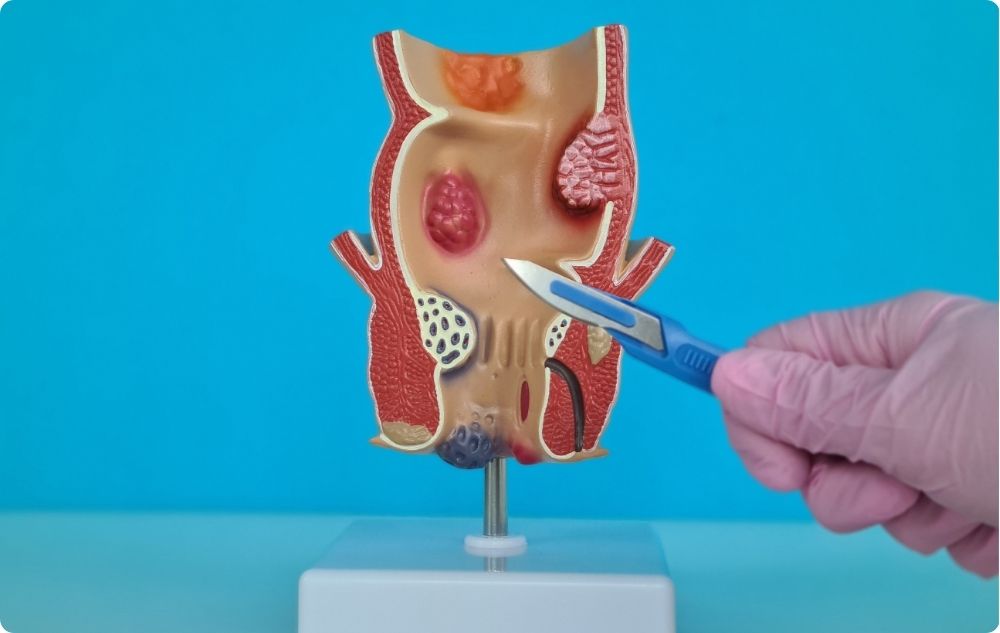
4. Degrees of Internal Hemorrhoids
Internal hemorrhoids develop progressively and go through four main grades/stages. Each grade is characterized by different symptoms, degree of discomfort and need for treatment.
Stage I - Initial stage

The hemorrhoids are still small and confined to the rectal canal. They do not appear outside the anus.
Symptoms:
- Mild and episodic bleeding during bowel movements;
- A feeling of mild discomfort or heaviness in the rectum;
- Itching due to mucus discharge;
- Absence of visible hemorrhoidal nodes;
- Without any symptoms, the condition is discovered accidentally during a routine examination.
At this stage, it is easiest to control the condition with lifestyle and dietary changes.
Stage II - Moderately advanced stage
Hemorrhoidal nodes protrude outside the anus during defecation, but retract spontaneously afterwards.
Symptoms:
- More frequent bleeding, especially with hard stools;
- Visible prolapse of the nodes during straining;
- Itching and irritation in the anal area;
- Slight leakage of mucus and moisture onto underwear;
- Foreign body sensation during defecation;
- Intermittent discomfort, worsening with prolonged sitting or physical exertion.
At this stage, treatment is more specific - it may include medications and minimally invasive procedures.
Stage III - Advanced stage
Hemorrhoids protrude from the anus during bowel movements or straining and do not retract on their own. Manual retraction is required.
Symptoms:
- More intense bleeding and a feeling of "bulging" around the anus;
- Need to manually retract after each bowel movement;
- Frequent feeling of pressure, tension and "fullness" in the rectum;
- Increased mucus secretion;
- Constant itching and irritation;
- Inflammation and swelling of the nodes;
- Painful sitting or physical activity.
It is difficult to rely solely on home remedies here. Specialized intervention such as ligation or sclerotherapy is often required.
Stage IV - Severe, chronic stage

Hemorrhoids are permanently outside the anus (they become External) and cannot be retracted, even manually. They can become trapped or inflamed.
Symptoms:
- A persistent bulge outside the anus, sometimes dark blue or purple in color;
- Sharp or throbbing pain, especially when pinched;
- Heavy bleeding with each bowel movement;
- Heavy mucus discharge, creating moisture and irritation;
- Risk of secondary infections, ulcers, or thrombosis;
- Impaired quality of life - pain when walking, sitting, wearing underwear;
- Social and emotional discomfort.
In most cases, this degree requires surgical intervention - classic surgery or modern techniques such as THD (transanal dearterization).
5. How long do Hemorrhoids last?
The duration of hemorrhoids depends on many factors - their type (Internal or External), the stage, the method of treatment, as well as the individual condition of the body. Some cases resolve quickly, while others become a chronic problem.
1. Acute hemorrhoids - from a few days to 2 weeks
Mild cases of Internal Hemorrhoids (Stage I) can resolve in 2-5 days with a proper diet and rest.
If measures are taken at the first symptoms - increased fiber intake, hydration, avoidance of stress - the symptoms decrease significantly within a week.
Without treatment, even mild cases can persist longer or progress to the next stage.
2. Moderate hemorrhoids - 1 to 4 weeks
In case of Internal hemorrhoids of stage II or III, the symptoms usually do not go away on their own.
When using topical medications (suppositories, ointments), warm baths, and proper diet, improvement occurs within 2-3 weeks.
If there is no improvement, minimally invasive procedures are recommended - they shorten the recovery period to 5-10 days after the intervention.
3. Chronic hemorrhoids - months or years
Stage III and IV Internal hemorrhoids that are left untreated can persist for a long time - even years.
Symptoms may occur periodically - with exacerbations during constipation, heavy meals, stress or prolonged standing.
In the chronic form, surgical treatment is often required, after which the recovery period is about 2 to 6 weeks.
4. After treatment - recovery and recurrence

With proper treatment, symptoms can disappear completely, but there is a risk of recurrence if lifestyle changes are not made.
Even after surgery, there is a need for long-term prevention: fiber, exercise, water, good hygiene.
The first 1-2 weeks after medical intervention are usually the most difficult, but full recovery is achieved within a month.
6. Treating Internal Hemorrhoids
Treatment for Internal Hemorrhoids depends on the stage of development, the frequency of symptoms, and the patient's general health. In most cases, the approach is stepwise - starting with milder measures and moving on to procedures and surgery if necessary.
Conservative treatment (initial approach)
This is the first stage of treatment and is mainly used for grade I and II internal hemorrhoids.
Lifestyle changes
- Increased fiber intake through fruits, vegetables, whole grains;
- Increase fluid intake - at least 2 liters daily;
- Avoiding prolonged sitting and physical exertion;
- Introducing moderate physical activity (walking, yoga, swimming).
Pharmacological agents
- Suppositories (suppositories) - contain substances to reduce inflammation and bleeding;
- Creams and ointments - relieve itching, cool and constrict blood vessels;
- Venotonics (tablets) - strengthen the venous wall and improve blood flow.
Warm sitz baths
- 10-15 minutes several times a day in lukewarm water - soothes the mucous membrane and reduces tension.
Minimally invasive procedures (without surgery)
These procedures are used for more stubborn hemorrhoids of stage II and III, when conservative treatment does not work.
Rubber Band Ligation
- The most commonly used method;
- A rubber ring is placed at the base of the hemorrhoid, which cuts off the blood supply;
- After a few days, the knot dries and falls off;
- The procedure is quick and almost painless, with a short recovery period.
Sclerotherapy
- Injection of a special solution that causes the walls of the veins to contract and stick together;
- Suitable for small to medium hemorrhoids;
- No need for anesthesia, performed on an outpatient basis.
Infrared coagulation
- A beam of infrared light is directed at the base of the hemorrhoid;
- The heat “seals” the blood vessel and the knot shrinks;
- The method is quick, but requires several sessions.
Surgical treatment (in severe or chronic cases)
In cases of stage III and IV or in the presence of complications, surgical treatment is most effective.
Hemorrhoidectomy (classic surgery)
- Removal of hemorrhoids by excision;
- Suitable for large or recurrent nodes;
- The most effective method, but with a longer recovery period (2-4 weeks).
THD (Transanal Hemorrhoidal Dearterialization)
- A modern technique that uses Doppler to locate and ligate the arteries feeding the hemorrhoids;
- Minimally invasive, with quick recovery and less pain.
Alternative and complementary therapies
- Phytotherapy - use of herbs with vein-strengthening and anti-inflammatory effects (horse chestnut, witch hazel);
- Homeopathy and natural products - used by some patients, but with variable effectiveness.
7. How to Prevent Internal Hemorrhoids
Prevention is the best treatment, although internal hemorrhoids often appear without warning, many of the risk factors can be controlled.
Here's what you can do to prevent them:
1. Create a healthy bowel movement routine
- Go to the toilet at the first urge - don't delay. Holding in stools leads to hardening;
- Don't spend more than 2-3 minutes on the toilet - avoid using your phone or reading, which prolongs your stay;
- Don't strain - if you need to strain, it's better to take a break and try again later.
2. Adjust your diet
- Include fiber in your diet every day - oats, lentils, apples, pumpkin, whole grain bread;
- Limit foods that cause constipation: white rice, white flour, fried and fatty foods;
- Avoid spicy spices - they irritate the mucous membrane and increase symptoms if you are predisposed;
- Maintain a regular diet - eating at the same time stimulates natural peristalsis.
3. Maintain good hydration

- Drink at least 1.5 - 2 liters of water per day - dehydration is a major factor in hard stools;
- Start the day with a glass of warm water - this activates the intestines and stimulates their movement;
- Avoid excessive consumption of coffee and alcohol - they have a diuretic effect and lead to fluid loss.
4. Exercise regularly
A sedentary lifestyle is a major risk factor. Include at least 30 minutes of exercise daily:
- Walking;
- Yoga;
- Light gymnastics
Avoid sitting for long periods of time - get up and move around every 45-60 minutes, especially when working in an office.
If you work in front of a computer, use a pillow with a hole (anti-hemorrhoidal) to reduce pressure on the rectum.
5. Maintain a healthy weight
- Excess weight increases pressure on the veins in the abdomen and pelvis;
- Even moderate weight loss can relieve the strain on the rectal veins;
- Avoid "yo-yo" diets - they disrupt normal bowel function.
6. Limit weight lifting
- Lifting heavy objects, especially without proper technique, leads to a sharp increase in intra-abdominal pressure;
- If physical exertion is required, inhale before lifting and exhale during the effort - this protects the abdomen from excessive pressure;
- With frequent exertion or physical labor, wear a stabilization belt.
7. Take care of your digestive system
- Use probiotics or yogurt with active cultures - they maintain the balance of intestinal flora;
- Avoid frequent use of laxatives - the body can "get used" to them and stop defecating on its own;
- After illness, antibiotics or stress - renew fiber and probiotics to restore normal bowel function.
8. Maintain intimate and anal hygiene

- Use soft toilet paper or wash with water after defecation;
- Avoid scented wet wipes - they contain chemicals that can irritate the area;
- Keep the area dry and clean - excessive moisture predisposes to irritation and inflammation.
8. Conclusion
Internal hemorrhoids are a widespread problem that can occur without clear symptoms or cause significant discomfort.
They go through different stages of development and require an individualized approach to treatment. Treatment options include both lifestyle changes and specialized medical interventions.
However, the best remedy against them remains prevention - through a balanced diet, exercise, good hygiene, and regular hydration.
SOURCES:
1. Webmd: Hemorrhoids: Symptoms, Causes, and Treatment (25.05.2024)
2. Healthline: Causes of Hemorrhoids and Tips for Prevention (25.05.2024)
3. Mayo Clinic: Hemorrhoids: Symptoms (25.05.2024)








